Tardbp Mutations in Individuals With Sporadic and Familial Amyotrophic Lateral Sclerosis.
- Inquiry commodity
- Open Access
- Published:
High frequency of the TARDBP p.M337 5 mutation among south-eastern Chinese patients with familial amyotrophic lateral sclerosis
BMC Neurology book 18, Article number:35 (2018) Cite this article
Abstract
Background
Amyotrophic lateral sclerosis (ALS) is a devastating motor neuron disease characterized by substantial clinical and genetic heterogeneity. Thus far, only a few TARDBP-ALS families have been reported in Red china, and no mutation assay has been reported in due south-eastern China.
Methods
Vii index cases from ALS families negative for SOD1 and FUS mutations were screened by Sanger sequencing for TARDBP gene exons ii-half dozen. TARDBP exon 6 was analysed in 215 sporadic ALS patients.
Results
Two TARDBP mutations in exon 6 (p.M337 V and p.G348C) were identified in 5 unrelated families. Four of these 5 families carried the same p.M337 5 mutation (family unit 1II3, family 2II6, family 3II4, and family 4II4), and the p.G348C mutation was identified in family unit v (II5). Among the 215 sporadic patients, just a single nucleotide polymorphism (p.A366A) was detected in 5 patients, and no responsible mutation was identified. Among the TARDBP-linked familial ALS patients, the average age of onset was 57.0 ± 4.seven years, and a trend towards higher rates of bulbar (l.0%, six/12) onset and upper limb (41.7%, 5/12) onset than lower rates of limb onset (8.3%, 1/12) was observed. Furthermore, ALS patients with TARDBP mutations showed a beneficial disease course, and the average survival was 106.five ± 41.8 months (northward = 8).
Conclusions
We found a high frequency of the TARDBP p.M337 V mutation in familial ALS in south-eastern China. The TARDBP-linked ALS patients showed a beneficial disease grade and prolonged survival.
Background
Amyotrophic lateral sclerosis (ALS) is a typical course of motor neuron disease characterized by selective degeneration of both the upper motor neurons (UMNs) and the lower motor neurons (LMNs) in the cerebral cortex, encephalon stalk, and spinal string, with an incidence of approximately i-ii per 100,000 people [ane]. Typically, ALS patients initially nowadays with symptoms in the upper limbs later in life (40-60 years old). The affliction then spreads to the torso and bulbar muscles, and patients ultimately die from respiratory failure, with a mean survival of 3-v years [2]. ALS is a progressive and incurable illness with no effective treatment available.
Currently, the complete aetiology of ALS is unclear. Approximately 5-10% of ALS patients have a family unit history of ALS (divers every bit familial ALS), and the remainder of patients have desultory ALS. ALS is a neurodegenerative disorder with substantial genetic heterogeneity, and more than thirty genes are associated with familial ALS. In the Caucasian population, chromosome 9 open reading frame 72 (C9ORF72, MIM: 614260) repeat expansions are the most mutual genetic cause of ALS; in China, Cu/Zn superoxide dismutase 1 (SOD1, MIM: 147450), fused in sarcoma/translated in liposarcoma (FUS/TLS, MIM: 137070), and TAR DNA-binding protein (TARDBP, MIM: 605078) are the primary causative genes amidst ALS patients [two, iii]. However, the frequencies of gene mutations are diverse between different populations, and this multifariousness has been linked to different genetic backgrounds. Thus far, simply a few TARDBP-ALS families have been reported in China, and no mutation assay has been reported in due south-eastern China [four,5,6,7].
In this study, 7 SOD1- and FUS-negative ALS families and 215 sporadic ALS patients were enrolled to screen the TARDBP mutation. Two TARDBP mutations in exon half-dozen (c.1009A > G, p.M337 5 and c.1042G > T, p.G348 C) were identified in five families (family 1II3, family 2II6, family 3II4, family 4II4, and family unit 5II5). Interestingly, iv unrelated ALS families (families 1-4) carried the same p.M337 5 mutation. No disease-causing mutations were identified in the sporadic ALS patients. TARDBP-linked familial ALS patients frequently showed upper limb and bulbar onset and had a benign illness grade.
Methods
Patients
Seven unrelated SOD1- and FUS-negative ALS families, including 13 ALS patients, were enrolled. All the families were of the Han ethnic group, were recruited from dissimilar regions of due south-eastern Prc, and had at least one affected family member. In addition, 215 sporadic ALS patients, including 148 males and 67 females, were enrolled in this written report. The average historic period at onset for desultory ALS was 54 ± 11.5 years. All the patients were diagnosed with possible, probable, or definite ALS co-ordinate to the revised EI Escorial criteria [8]. The patients were recruited from the Section of Neurology, First Affiliated Hospital of Fujian Medical University from August 2008 to August 2016. Clinical profiles, including the age at onset, site at onset, disease class, laboratory data, electromyography (EMG) results, motor part, and pulmonary function, were analysed.
Gene mutation analysis
Genomic DNA was extracted from peripheral blood using a Genomic Extraction Kit (Qiagen, Germany). First, the survival of motor neuron gene (SMN1 and SMN2, MIM: 600354) mutations were screened to exclude the possibility of spinal muscular atrophy (SMA). For the male patients, CAG expansion in the androgen receptor factor (AR, MIM: 313700) was further detected to exclude spinal and bulbar muscular cloudburst (SBMA). The patients negative for mutations in the SMN and AR genes were then selected for ALS gene screening. SOD1- and FUS-negative familial ALS patients were selected to screen for TARDBP cistron mutations by Sanger sequencing, and the primer sequences are listed in Additional file 1: Table S1.
Results
Gene mutation analysis of the ALS patient cohort
Amongst the seven unrelated SOD1- and FUS-negative ALS families, we identified 2 known TARDBP mutations (TARDBP: c.1009A > G, p.M337 V and TARDBP: c.1042G > T, p.G348C) in v families. Interestingly, the TARDBP: c.1009A > Chiliad, p.M337 Five mutation was found in family ane, family 2, family 3, and family 4 (Fig. one). Among the 215 sporadic patients, five patients carried a heterozygous variant (c.1098C > M, p.A366A), which was confirmed to be a single nucleotide polymorphism. Withal, no responsible gene mutation was identified in exon vi of the TARDBP factor for this cohort of sporadic patients.
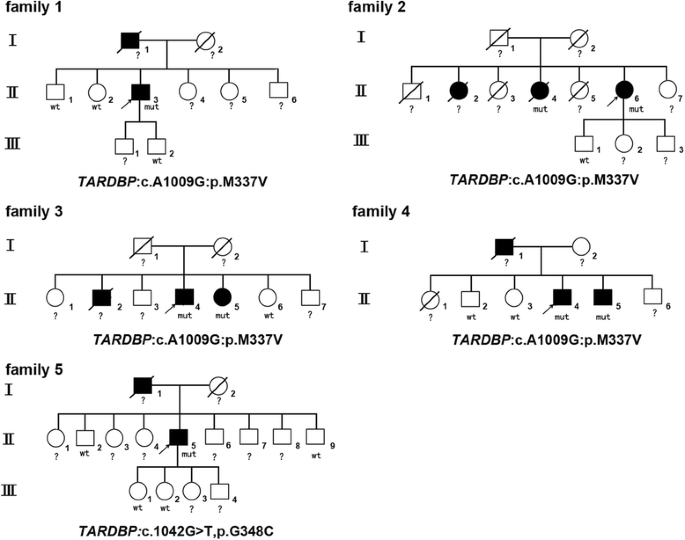
Pedigrees and gene mutations of the v ALS families. The squares represent males. The circles represent females. The black symbols represent affected patients. The arrows signal the probands. The diagonal lines across symbols represent deceased patients. "mut" indicates the afflicted carriers of the gene mutation. "wt" indicates healthy family members without the gene mutation. "?" indicates an undetected gene mutation due to subject decease or refusal to participate in further genetic analysis
Clinical features of four pedigrees with the TARDBP c.1009A > G, p.M337 V mutation
Offset at 58 years of age, the proband of family 1 (II3) developed progressive speech and swallowing difficulties. Initially, he was diagnosed with vocal cord polyps in the ear-nose-throat department and underwent vocal cord polypectomy. However, his symptoms did not resolve and gradually worsened. Muscular weakness and atrophy spread to his upper limbs and and so to his lower limbs. Neurological exam indicated mild muscle atrophy in his tongue and limbs with increased tendon reflexes and the Chaddock sign bilaterally. EMG testing revealed widespread neurogenic lesions. He died from respiratory failure nine years afterwards. His father (I1) also suffered from similar symptoms and died vi years after symptom onset.
The proband of family 2 (II6) was a 61-year-old female who suffered from right upper limb stiffness and weakness for ii years. I year later on, she developed swallowing and speaking difficulties. Neurological exam showed dysarthria and choking. Musculus weakness was constitute in the neck flexor muscle (grade 4) and correct limbs (grade 5-) without significant muscle atrophy. The jaw reflex and Babinski sign were positive. EMG revealed widespread neurogenic lesions in the sternocleidomastoid and the cervical, lumbar, and thoracic paraspinal muscles (T8). Her older sister (II2) also developed dysarthria at lx years of age and died 12 years later. Another sister (II6) showed speaking and swallowing difficulties beginning at 58 years of age. Her symptoms progressed, and limb muscle weakness and cloudburst were noted after 1 year. EMG testing also revealed widespread neurogenic lesions. She was diagnosed with bulbar-onset ALS and died from respiratory failure afterwards surviving for 120 months.
The proband of family 3 (II4) was a male person patient who developed muscle weakness in the correct upper limb at the age of 62 years that spread to the left upper limb and bulbar muscles 2 years later. Neurological exam showed meaning musculus atrophy in the bilateral mitt muscles, including the interosseous and thenar muscles. Mild muscle weakness (grade v-) was detected in the limbs with increased tendon reflexes bilaterally. Neurogenic lesions were observed in the muscles innervated by the cervical, lumbar, and thoracic (T8, T9, and T10) spinal cord. His sis (II5) was also admitted to our department and presented with muscle weakness in her lower left limb 8 months prior to admission and developed speaking difficulties and choking two months later. Neurological examination showed mild muscle weakness (grade five-) in the neck and lower limb muscles without musculus weakness. Hypermyotonia was observed in the upper and lower left limbs. Tendon reflexes were significantly increased in all the limbs. Additionally, the Hoffmann and Babinski signs were positive. EMG testing revealed widespread neurogenic lesions. At the age of 50 years, his older brother (II2) suffered from musculus weakness in the upper limbs that spread to his bulbar muscles. He was too diagnosed with ALS and died due to respiratory failure 3 years later.
The proband of family four (II4) was a 59-year-erstwhile male who adult dysarthria at 54 years of age. In the years post-obit symptom onset, his symptoms slowly progressed, and the affected limb muscles caused walking and writing abnormalities. Neurological exam showed muscular fasciculation without pregnant muscle atrophy. The tendon reflexes were increased in all the limbs. The Chaddock sign and palm-chin reflex were positive bilaterally. EMG testing revealed widespread neurogenic lesions. His begetter (I1) developed dysarthria at the age of 62 years and died 14 years later on. His younger brother (II5) likewise carried the TARDBP c.1009A > G, p.M337 Five mutation; however, he presented with no noticeable symptoms until recently.
Clinical features of the pedigree with the TARDBP c.1042G > T, p.G348C mutation
The proband of family unit 5 (II5) was a 55-year-old male who start presented with muscle weakness and atrophy in his correct hand at fifty years old. Ii years later, his symptoms progressed to the left side, and he reported difficulty in raising his hands. Iii years later, weakness and atrophy as well developed in his lower limbs. Currently, he cannot walk unassisted. Neurological examination showed significant muscle weakness (grade 2-iii) and cloudburst in the upper and lower limbs without UMN signs. EMG revealed widespread neurogenic lesions. His begetter (I1) also presented with upper limb weakness at 50 years old and died 10 years later.
Discussion
In this report, among the seven unrelated SOD1- and FUS-negative ALS families, we detected 2 TARDBP mutations (c.1009A > One thousand, p.M337 Five and c.1042G > T, p.G348C) in 5 families. Importantly, 4 families carried the same TARDBP mutation, c.1009A > G, p.M337 V. Hou Fifty et al. screened SOD1, TARDBP, and FUS gene mutations in ALS patients from primal-southern China and revealed that SOD1 (20%) and FUS (13.3%) mutations were the principal causal mutations in familial ALS, only they did not detect whatsoever TARDBP-linked ALS families [9]. In a Brazilian research centre, Chadi G et al. reported that the most common gene mutations in familial ALS were VAPB (43.six%), C9orf72 (12.8%), and SOD1 (7.vii%), whereas no FUS or TARDBP mutations were detected in whatever familial ALS subjects [10]. In Australia, McCann EP et al. also reported that the main factor mutations in familial ALS were SOD1 (13.7%), FUS (2.4%), and TARDBP (ane.9%) [11]. Our study indicated a loftier frequency of the TARDBP gene mutation in familial ALS in the south-eastern region of Communist china.
Amid the five ALS families with the TARDBP gene mutation in the present study, 12 symptomatic ALS patients and one asymptomatic patient were identified (Table one). For the 12 symptomatic patients, including 8 males and 4 females, the average age of onset was 57.0 ± iv.7 years. In addition, the TARDBP-linked familial ALS patients presented a trend towards higher rates of bulbar (fifty.0%, 6/12) onset and upper limb (41.7%, 5/12) onset than lower rates of limb onset (eight.3%, 1/12); this finding is consistent with a predominance of upper limb onset in TARDBP-linked ALS reported in a previous report [12]. Furthermore, similar to previous reports, ALS patients with TARDBP mutations showed a beneficial illness form and an average survival of 106.v ± 41.eight months (due north = eight) [13].
Furthermore, TARDBP p.M337 V ALS patients showed substantial clinical heterogeneity between and among families carrying the same mutation. These patients could exhibit a LMN-ascendant presentation, an UMN-dominant presentation, or the typical presentation with both LMN and UMN involvement, which is similar to the cases that we reported in family 2 and family 3. In addition, in family iii, compared with affected members II4 and II5, II2 offset showed symptoms at the age of 50 years and died from respiratory failure 36 months after, reflecting a relatively short illness elapsing, which may advise intrafamilial clinical heterogeneity. We as well establish a p.M337 V carrier without any neurological symptoms in family 4, which may be explained by incomplete penetrance; no like patient has been previously reported. In improver, Ju X et al. reported a full-blooded with the p.M337 5 mutation that showed cerebral impairment. In this study, none of the 4 families with the p.M337 V mutation developed cognitive impairment; this result is similar to the results from a Taiwanese accomplice. The substantial clinical heterogeneity betwixt p.M337 V mutation pedigrees indicated the potential presence of other underlying phenotype-modifying factors [14, fifteen]. Kühnlein P et al. described the starting time ALS patient with the p.G348C mutation who presented with early spinal onset (31 years) without cerebral impairment [xvi]. Del Bo R et al. as well reported a five-generation p.G348C mutation ALS family with ix afflicted members, and the affected members showed highly variable clinical features, including the age at onset (36 to 67 years) and disease elapsing (36 to sixty months) [17]. In this study, p.G348C mutation ALS patients (family unit v, I1 and II5) had an age of onset of 50 to 55 years and spinal onset, which are similar to the features of previously reported patients [sixteen, 17]. Among different ethnic groups, due to different genetic backgrounds, patients with TARDBP gene mutations also show substantial clinical heterogeneity. According to Corcia P et al., approximately 51.3% of Caucasian ALS patients have upper limb onset, while 58.8% of Asian patients take bulbar onset [18]. Similarly, bulbar-onset patients accounted for 50% of the patients in this study.
In this report, only a single nucleotide polymorphism (c.1098C > G, p.A366A) was identified in 5 sporadic patients. However, no mutation was detected in exon 6 of the TARDBP gene in the 215 sporadic patients. Similarly, in southern China, Ye CH et al. detected no TARDBP exon half-dozen mutations in 207 sporadic ALS patients [nineteen]. Huang R and Zou ZY demonstrated that the frequency of TARDBP gene mutations in Chinese desultory ALS patients was approximately 0.61% to 0.73% [5, 20]. The c.1098C > Grand, p.A366A polymorphism, which may increment susceptibility to ALS, was also previously reported [5].
Conclusions
TARDBP gene mutations are the common causal mutations in this accomplice of familial ALS patients from due south-eastern China, with a loftier frequency of the p.M337 V mutation. The TARDBP-linked ALS patients showed substantial clinical heterogeneity and a more benign affliction phenotype with a longer illness duration.
Abbreviations
- ALS:
-
Amyotrophic lateral sclerosis
- AR :
-
Androgen receptor gene
- C9ORF72 :
-
Chromosome nine open reading frame 72 repeat expansion
- FUS/TLS :
-
Fused in sarcoma/translated in liposarcoma
- LMN:
-
Lower motor neuron
- SBMA:
-
Spinal and bulbar muscular cloudburst
- SMA:
-
Spinal muscular atrophy
- SMN :
-
Survival of motor neuron gene
- SOD1 :
-
Cu/Zn superoxide dismutase ane
- TARDBP :
-
TAR DNA-bounden protein
- UMN:
-
Upper motor neuron
References
-
Logroscino G, Traynor BJ, Hardiman O, Chiò A, Mitchell D, Swingler RJ, Millul A, Benn East, Beghi East. EURALS. Incidence of amyotrophic lateral sclerosis in Europe. J Neurol Neurosurg Psychiatry. 2010;81:385–90.
-
Li HF, Wu ZY. Genotype-phenotype correlations of amyotrophic lateral sclerosis. Transl Neurodegener. 2016;5:iii.
-
Zou ZY, Zhou ZR, Che CH, Liu CY, He RL, Huang HP. Genetic epidemiology of amyotrophic lateral sclerosis: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2017; https://doi.org/10.1136/jnnp-2016-315018.
-
Tsai CP, Soong BW, Lin KP, Tu PH, Lin JL, Lee YC. FUS, TARDBP, and SOD1 mutations in a Taiwanese cohort with familial ALS. Neurobiol Aging. 2011;32:553. e13-21
-
Zou ZY, Peng Y, Wang XN, Liu MS, Li XG, Cui LY. Screening of the TARDBP gene in familial and sporadic amyotrophic lateral sclerosis patients of Chinese origin. Neurobiol Aging. 2012;33:2229. e11-2229.e18
-
Ju 10, Liu W, Li X, Liu N, Zhang N, Liu T, Deng M. Two distinct clinical features and cognitive impairment in amyotrophic lateral sclerosis patients with TARDBP factor mutations in the Chinese population. Neurobiol Aging. 2016;38:216. e1-6
-
Liu ZJ, Lin HX, Liu GL, Tao QQ, Ni W, Xiao BG, Wu ZY. The investigation of genetic and clinical features in Chinese patients with juvenile amyotrophic lateral sclerosis. Clin Genet. 2017; https://doi.org/x.1111/cge.13015.
-
Brooks BR, Miller RG, Swash M, Munsat TL, World Federation of Neurology Inquiry Group on Motor Neuron Diseases. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotrop Lateral Scler. 2000;one:293–9.
-
Hou L, Jiao B, Xiao T, Zhou L, Zhou Z, Du J, Yan X, Wang J, Tang B, Shen L. Screening of SOD1, FUS and TARDBP genes in patients with amyotrophic lateral sclerosis in Cardinal-Southern People's republic of china. Sci Rep. 2016;6:32478.
-
Chadi G, Maximino JR, Jorge FMH, Borba FC, Gilio JM, Callegaro D, Lopes CG, SND Southward, GNS R. Genetic assay of patients with familial and sporadic amyotrophic lateral sclerosis in a Brazilian research center. Amyotroph Lateral Scler Frontotemporal Degener. 2017;18:249–55.
-
McCann EP, Williams KL, Fifita JA, Tarr IS, O'Connor J, Rowe DB, Nicholson GA, Blair IP. The genotype-phenotype landscape of familial amyotrophic lateral sclerosis in Australia. Clin Genet. 2017;92:259–66.
-
Millecamps S, Salachas F, Cazeneuve C, Gordon P, Bricka B, Camuzat A, Guillot-Noël L, Russaouen O, Bruneteau G, Pradat PF, Le Forestier N, Vandenberghe N, Danel-Brunaud V, Guy N, Thauvin-Robinet C, Lacomblez 50, Couratier P, Hannequin D, Seilhean D, Le Ber I, Corcia P, Camu W, Brice A, Rouleau K, LeGuern E, Meininger Five. SOD1, ANG, VAPB, TARDBP, and FUS mutations in familial amyotrophic lateral sclerosis: genotype-phenotype correlations. J Med Genet. 2010;47:554–60.
-
Sreedharan J, Blair IP, Tripathi VB, Hu X, Vance C, Rogelj B, Ackerley Southward, Durnall JC, Williams KL, Buratti E, Baralle F, de Belleroche J, Mitchell JD, Leigh PN, Al-Chalabi A, Miller CC, Nicholson 1000, Shaw CE. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319:1668–72.
-
Piaceri I, Del Mastio M, Tedde A, Bagnoli South, Latorraca S, Massaro F, Paganini Thousand, Corrado A, Sorbi S, Nacmias B. Clinical heterogeneity in Italian patients with amyotrophic lateral sclerosis. Clin Genet. 2012;82:83–seven.
-
Borghero G, Pugliatti M, Marrosu F, Marrosu MG, Murru MR, Floris Thousand, Cannas A, Parish LD, Occhineri P, Cau TB, Loi D, Ticca A, Traccis Southward, Manera U, Canosa A, Moglia C, Calvo A, Barberis M, Brunetti M, Pliner HA, Renton AE, Nalls MA, Traynor BJ, Restagno G, Chiò A, ITALSGEN and SARDINALS Consortia. Genetic architecture of ALS in Sardinia. Neurobiol Crumbling. 2014;35:2882. e7-2882.e12
-
Kühnlein P, Sperfeld AD, Vanmassenhove B, Van Deerlin V, Lee VM, Trojanowski JQ, Kretzschmar HA, Ludolph AC, Neumann M. Two German kindreds with familial amyotrophic lateral sclerosis due to TARDBP mutations. Curvation Neurol. 2008;65(nine):1185–9.
-
Del Bo R, Ghezzi S, Corti Southward, Pandolfo One thousand, Ranieri M, Santoro D, Ghione I, Prelle A, Orsetti Five, Mancuso M, Sorarù Thousand, Briani C, Angelini C, Siciliano Yard, Bresolin Due north, Comi GP. TARDBP (TDP-43) sequence analysis in patients with familial and sporadic ALS: identification of two novel mutations. Eur J Neurol. 2009;16:727–32.
-
Corcia P, Valdmanis P, Millecamps Southward, Lionnet C, Blasco H, Mouzat 1000, Daoud H, Belzil V, Morales R, Pageot N, Danel-Brunaud V, Vandenberghe N, Pradat PF, Couratier P, Salachas F, Lumbroso S, Rouleau GA, Meininger V, Camu W. Phenotype and genotype analysis in amyotrophic lateral sclerosis with TARDBP gene mutations. Neurology. 2012;78:1519–26.
-
Ye CH, Lu 40, Zheng MY, Zhen J, Li ZP, Shi L, Liu ZY, Feng LY, Pei Z, Yao XL. Absence of mutations in exon half-dozen of the TARDBP gene in 207 Chinese patients with sporadic amyotrohic lateral sclerosis. PLoS One. 2013;8:e68106.
-
Huang R, Fang DF, Ma MY, Guo XY, Zhao B, Zeng Y, Zhou D, Yang Y, Shang HF. TARDBP gene mutations among Chinese patients with sporadic amyotrophic lateral sclerosis. Neurobiol Aging. 2012;33:1015. e1-6
Acknowledgements
The authors sincerely thank the ALS patients for their aid and willingness to participate in this study.
Funding
This work was supported by grants U1505222 (Ning Wang) and 81701133 (Qi-Jie Zhang) from the National Natural Science Foundation of China and the National Key Clinical Specialty Bailiwick Construction Program and Key Clinical Specialty Field of study Construction Programme of Fujian.
Availability of information and materials
Study data are available from the corresponding author upon reasonable request.
Author data
Affiliations
Contributions
Study concept and design (WJC, NW and QJZ); acquisition and estimation of the data (GRX, WH, LLZ, CW, LQX, MTL, and QJZ); drafting of the manuscript (QJZ, GRX, and WH); critical revision of the manuscript for important intellectual content (QJZ, WJC, and NW); conquering of funding (QJZ and NW); administrative, technical, or material support (GRX, WH, LLZ, CW, LQX, and MTL); study supervision (QJZ and NW). All the authors read and approved the final manuscript.
Respective authors
Ethics declarations
Ethics approval and consent to participate
This study was canonical by the Ethics Board of First Affiliated Hospital of Fujian Medical University. Written informed consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they take no competing interests.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Rights and permissions
Open Access This commodity is distributed under the terms of the Creative Eatables Attribution 4.0 International License (http://creativecommons.org/licenses/past/4.0/), which permits unrestricted apply, distribution, and reproduction in whatsoever medium, provided you give appropriate credit to the original writer(due south) and the source, provide a link to the Artistic Commons license, and bespeak if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made bachelor in this article, unless otherwise stated.
Reprints and Permissions
About this commodity
Cite this article
Xu, Gr., Hu, West., Zhan, LL. et al. Loftier frequency of the TARDBP p.M337 V mutation amid south-eastern Chinese patients with familial amyotrophic lateral sclerosis. BMC Neurol 18, 35 (2018). https://doi.org/10.1186/s12883-018-1028-1
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12883-018-1028-i
Keywords
- Amyotrophic lateral sclerosis
- Familial
- TARDBP
- Genotype-phenotype assay
Source: https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-018-1028-1
Posting Komentar untuk "Tardbp Mutations in Individuals With Sporadic and Familial Amyotrophic Lateral Sclerosis."